Our well-being is uniquely tied to the condition of our colon, which is commonly unhealthy at diagnosis of celiac disease. To keep our colon healthy, we need to understand what happens there on a microscopic level. Hundreds of varieties of intestinal microbe populations called “flora” live there, numbering in the billions. To put these numbers into focus, dead bacteria make up about a third of each bowel movement. Our resident microbes, whether beneficial or harmful, play a decisive role in nourishing or damaging the cells that form the intestinal lining. Probiotic and prebiotic foods and supplements restore and feed our friendly microbes.
Probiotics are microbial foods or supplements that can be used to change or reestablish the intestinal flora to improve the health of the host (us). Prebiotics are non-digestible food products that stimulate the growth of symbiotic bacterial species, present in the colon, that improve the health of the host, according to the World Health Organization definition. Symbiotic means the flora get nourishment from us and we get nourishment from them.
In celiac disease, there are serious reasons to respect probiotic and prebiotic foods and supplements. Intestinal enzyme deficiencies, sugar intolerances and associated dysbiosis, or imbalance of intestinal flora, appear commonly.1 Research indicates that the metabolic activity of flora in celiacs is different from the general population and that it is a genuine phenomenon of celiac disease not affected by either the diet, the inflammation, or the autoimmune status of the patient.2 In addition, the severity of disturbances in intestinal balance of flora was found to depend on the gravity of the patient’s state.3
Before treatment with a gluten-free diet, the immune reaction within the small intestinal lining causes inflammation and damage to the delicate structures of the lining, leading to failure to digest and absorb nutrients. Unabsorbed nutrients pass into the colon where their unnaturally large presence brings about colon dysfunction with stool changes.
The arrival of large quantities of undigested fat, carbohydrates and protein into the colon along with poor gut motility and certain nutrient deficiencies cause microbial imbalances in these ways:
1. Maldigestion results from pancreatic insufficiency, bile insufficiency and digestive enzyme deficiencies. Pancreatic insufficiency means the pancreas cannot produce enough of the digestive enzymes lipase needed for the digestion of fat, amylase needed for the digestion of carbohydrates, and protease needed for the digestion of protein. Bile insufficiency results in impaired secretion of bile by the liver, obstruction of the bile ducts that carry bile and abnormal circulation of bile salts that impairs the digestion of fats. Deficiency of lactase, sucrase, and maltase enzymes in the villi, microscopic absorbing structures of the small intestinal lining, results in failure to finish the digestion of sugars. Deficiency of protease enzymes in the microscopic villi results in failure to finish the digestion of protein required for absorption into the bloodstream.
Undigested carbohyrates arriving in the colon cause excessive fermentation and draw water from the bloodstream into the colon. These conditions produce symptoms such as abdominal pain, watery diarrhea, IBS-like symptoms, bloating, and gas. Pale foul-smelling stool that float or stick to the toilet bowl results from fat malabsorption. Protein maldigestion encourages putrefaction.
2. Altered gut motility, or movement of food through the digestive tract, and low stomach acidity commonly found in celiac disease promote excessive fermentation in the large bowel and overgrowth of yeast and bacteria in the small bowel, both serious conditions.
3. The health and integrity of intestinal cells depends on adequate availability of thiamin, riboflavin, niacin, zinc and vitamin A. Deficiency of these nutrients sets the stage for inflammation, infection and diarrhea that worsen gut function and induce overpopulation by pathogens, disease-producing microbes. Magnesium and potassium are needed for muscle contraction.
How probiotic flora improve health.
Probiotic flora inhibit colonization of pathogens by physically preventing them from adhering to the gut lining. Other important functions are:
- Produce short chain fatty acids (SCFA)s as propionic, acetic, i-butyric,and i-valeric acid. SCFAs are important and necessary energy byproducts formed during fermentation of undigested carbohydrates in the colon by flora. SCFAs nourish the colonocytes, the cells that line the colon. They also help absorb salts and water from stool.
- Produce a form of vitamin K and appreciable amounts of biotin.
- Reduce the presence of putrefactive enzymes.
- Protect against toxic substances, such as heavy metals.
- Contribute to normal bowel movements.
For these reasons, we need to use probiotics and prebiotics every day to improve our overall health and specifically our intestinal health. This is especially important if fatigue, weakness, achiness, depression, foggy thinking and digestive problems continue while maintaining a gluten-free diet.
Sources
Good probiotic food sources to replace lost or reduced flora in the colon include fermented products such as yogurt, kefir, sauerkraut, miso, and unpasteurized apple cider vinegar.
Probiotic supplements that are guaranteed to contain billions of live organisms, such as lactobacillus and bifidobacillus, are very helpful to quickly establish or renew flora. In addition, lactobacillus and bifidobacillus make the colon more acidic, which keeps harmful microbes such as Candida albicans, a yeast, from living and multiplying.
Prebiotics include dietary fiber and fructo-oligosaccharides (FOS). FOS are simple sugars called neosugars, partly composed of fructose, that cannot be digested in the small intestine therefore passing into the colon. In the colon, they stimulate the growth of beneficial bacteria including bifidobacteria and lactobacillus, which results in the reduction of harmful bacteria, such as salmonella and clostridia. One study revealed that increasing these neosugars causes an increase in bifidobacteria and a decrease in the activity of ß-glucuronidase, an enzyme which converts procarcinogens to carcinogens in the bowel. Carcinogens are able to induce cancer.
Food sources of FOS include honey, gluten-free beer, onion, burdock root, asparagus, Jerusalem artichoke, banana, maple sugar, and Chinese chives.
Natural foods that improve digestion and movement of food through the digestive tract include raspberry, celery, lemon, horseradish, carrot, grapes, lettuce, onions, garlic, cinnamon and ginger.
In summary, probiotics and prebiotics with support of a daily 100% vitamin/mineral supplement can help us recover faster and more fully on the gluten-free diet and maintain health.
References:
- Tjellström B, Stenhammar L, Högberg L, Fälth-
Magnusson, K Magnusson KE, Midtvedt T,
Sundqvist T, Norin E. Gut microflora associated characteristics in children with celiac disease.
Scand J Gastroenterol. 2001 Feb;36(2):163-8. - Murray IA, Smith JA, Coupland K, Ansell ID,
Long RG. Intestinal disaccharidase deficiency
without villous atrophy may represent early
celiac disease. Am J Gastroenterol. 2005 Dec;
100(12):2784-8 - Kamilova AT, Akhmedov NN, Nurmatov BA.
Intestinal microbiocenosis in children with
intestinal enzymopathy. Zh Mikrobiol
Epidemiol Immunobiol. 2001 May-Jun;
(3):97-9. - Kathleen Mahan and Sylvia Escott-Stump,
ed, Krause’s Food, Nutrition, and Diet Therapy.
10th Edition. Philadelphia,USA: WB Saunders
Company, 2000, p. 278.Copyright © Cleo Libonati 2007.
——————————-
Cleo Libonati, Philadelphia, PA, USA
President/CEO of Gluten Free Works, Inc.
Author, Recognizing Celiac Disease
Cleo Libonati Email
 Gluten Free Works Gluten Free Resources News and Tips
Gluten Free Works Gluten Free Resources News and Tips



Great information :)
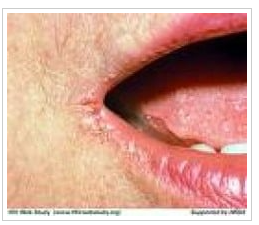
I used to be 95lbs and at 5’5″ that’s not healthy of course. All food went straight through me. I was very malnourished and my nerves were shot. I could barely climb the stairs without resting. One bite with glutens made me very ill. I had dermatitis herpeitformis all over my elbows and shins. It was uneblieveably ithchy and I scratched until I bled, despite steroid creams.
I went to a ton of doctors. Celiac tests were negative. I was diagnosed as depressed (who wouldn’t be).
Anyway, I did a lot of research, discovered antibiotics had killed the bacteria that creates the slime that protects your intestines from stomach acid and us a food transporter to your villi and that these bacteria are in unpasteurized milk (which is illegal to sell).
The stomach acids burn holes in your intestines and leads to leaky gut and IBS (which I had terribly – I dreaded eating because it meant long painful session in the bathroom). Undigested proteins from glutens enter the blood stream and set off an auto immune response because they appear foreign invaders to the immune system. I developed inflammatory arthritis and skin rashes.
I was sick like this for about 30 years. Everyone thought I was bulimic or just not eating (everything I ate was the highest nutrition and fat content and I took tons of vitamins) and it was very disheartening. My hair fell out eventually in patches, my teeth were wobbly, my skin was blotchy, my breath was nasty no matter what I did, I was very weak and eventually my nerves just broke and I started having panic attacks – a sypmton of a variety of nutritional deficiencies but very importantly – niacin (which is abundant in Cheetos which I love). I also started menopause at 45 yrs old which is early. The hair loss was probably due to copper deficiency. I looked awful. I felt awful.
I reverse the menopause constant hot flashes with bio identical hormone replacement therapy. I don’t seem to need it now. My periods came back. I’m nearly 50.
Anyway, I discovered probiotics and juicing and started taking Udo’s Choice and Natural Factors probiotic brands. I also started eating live yogurt which I got from the Hutterites as a gift. I made my own yogurt from their starter cultures. You can buy it now of course.
I started feeling better almost within days. It was amazing. I called a friend when I did my first solid poop in years – I knew that meant I was recovering – finally.
I am now fully recovered but still eat yogurt and kefir and take capsule probiotic from time to time. I also juice a lot because nutrient deficiencies are much more quickly resolved with kale, carrot. apple and celery etc than with vitamin pills (which I still take for vitamin D and curcumin for other reasons you should google if you have cancer or are at high risk. I also take milk thistle because my liver took a beating when I was ill. My doctor refused to believe I don’t drink and just assumed I was lying. Celiacs are at high risk of pancreatic and liver cancer not surprisingly. I choose organic products for the higher nutrient content and lack of chemical sprays.
Mixing kefir and fresh juices soothes my stomach and helps the bacteria grow.
I weigh 128lbs and look and feel amazing. People who didn’t see me from when I was sick to when I really put on weight and got color in may face didn’t recognize me sometimes. A few people had to do a double take.
The irony of this story is that my mother used to make yogurt when I was a kid and she insisted it would soothe an upset tummy and put bacteria back in us if we took antibiotics as kids. I didn’t really understand. She was right of course. That’s old knowledge women have known for centuries but ignored by modern medicine. Remember before modern medicine, women gathered the herbs and medicines and made the food and nursed the sick. They held that body of knowledge which as largely dismissed as old wives tales by the men who industrialized modern medicine later.
Once I left home I didn’t get any more of mom’s yogurt and that’s when I got really ill on a steady decline of bronchial infections and antibiotics. She used to nag me to eat yogurt but I don’t think I did very often and I doubt it had a lot of live cultures in it. It would have saved so much trouble.
I hope others relate to my story and get better too. It’s really not difficult.
Great article and Libby also raises an interesting possibility: that prior to gluten auto-immune response and fermenting undigested food in colon, excess stomach acid (gastritis) induced by antibiotics, has caused leaky gut and hence the opening for glutens into the bloodstream. Would be interested if anyone can collaborate this hypothesis with scientific evidence.